Decades of brain imaging have failed to surface reproducible signatures of autism and other psychiatric conditions, and a new study may explain why: The specific brain areas that are smaller or larger than usual differ across people who share any one of six diagnoses, but those areas tend to connect via overlapping circuits and networks, according to the new work.
The finding “drives home a point that we’ve been skirting around for many, many years,” says Lucina Uddin, professor of psychiatry and biobehavioral sciences at the University of California, Los Angeles, who was not involved with the work. “It’s not likely that we’ll find one or even a couple of brain regions that are the area of dysfunction in any of these disorders, because it’s more likely that there’s big kind of large-scale systems that are dysfunctional in slightly different ways.”
The brain changes associated with individual conditions, including attention-deficit/hyperactivity disorder, autism and schizophrenia, are notoriously variable, previous studies have shown. But the amount of variance from person to person, and whether the associated circuits also show heterogeneity, has been unclear.
To get at this question, the researchers pored over data from 14 MRI studies collected across 25 sites to obtain gray-matter volume measurements for about 1,000 brain areas in 1,294 adults with ADHD, autism, bipolar disorder, major depressive disorder, obsessive-compulsive disorder or schizophrenia, and 1,465 people without any of these conditions.
Instead of comparing the average volume of each area across groups of participants, the team used an approach called normative modeling, comparing the volumes in each participant who had a psychiatric condition with the typical volumes across those who did not have a psychiatric condition.
“It’s [a] much more nuanced approach,” says Maria di Biase, a senior research fellow in psychiatry at the University of Melbourne in Australia, who was not involved with the study.
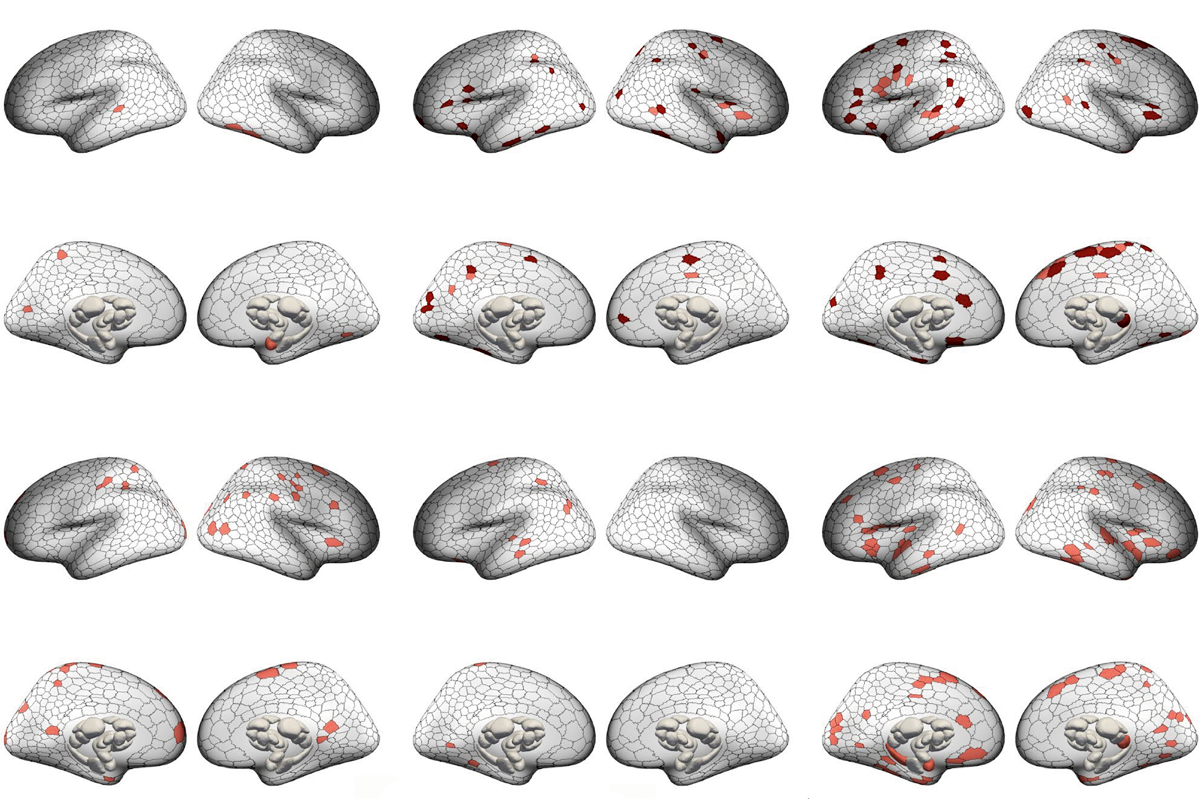
The participants with a psychiatric condition showed several unusually large or small brain areas, the study found, but the affected areas differed across people with a given condition. Only about 3 to 7 percent of people across all conditions showed brain changes within the same area, highlighting the heterogeneity of psychiatric conditions. For example, only 5 percent of people with autism had similar brain regions affected.
“[These findings] call [into] question our long history of comparing a group of patients to a group of controls, because it suggests that we can’t simply lump all patients together, since the neurobiology underlying these disorders may differ between patients,” di Biase says.
Even though the affected regions in each condition varied, they typically formed connected circuits, the researchers found. These circuits overlapped in about 39 to 50 percent of participants in each diagnostic group, compared with a 33 percent overlap among controls.
The brain regions altered in each condition were usually embedded within the same functional networks, the study also shows. For example, a network called the salience network, which helps direct attention, was implicated in all of the conditions included in the study except autism. The results were published in August in Nature Neuroscience.
“Targeting circuits, rather than specific brain regions, may be a more effective way of developing treatments,” says study investigator Ashlea Segal, who is now a postdoctoral research fellow at Yale University.
Interestingly, the participants with autism had many brain areas that were larger than usual, whereas people with the other conditions had many brain areas that were smaller. Many of the enlarged circuits lie within the visual, parietal and frontal cortices, which may reflect previously reported accelerated brain growth in people with autism.
The findings also make a case for personalized medicine and the need to understand the brain alterations in each person, says Alex Fornito, professor of psychological sciences at Monash University in Melbourne, Australia, who led the work. For example, about one-third of study participants with depression or bipolar disorder showed alterations in one particular circuit in the prefrontal cortex, which is already targeted in those who undergo brain stimulation as a treatment.
“That means we need to identify new targets for the other two-thirds of people,” Fornito says. “Ultimately, if we’re going to develop tailored treatments, we need to understand individual variability.”
The next step, Uddin says, is to understand exactly how the overlapping circuits and networks could underlie certain traits of the psychiatric conditions. “[The study] highlights how important it is to think at the circuit level and think broader than ‘one brain region, one function,’” she says. “Because we know that just isn’t how things are set up.”
This content was originally published here.