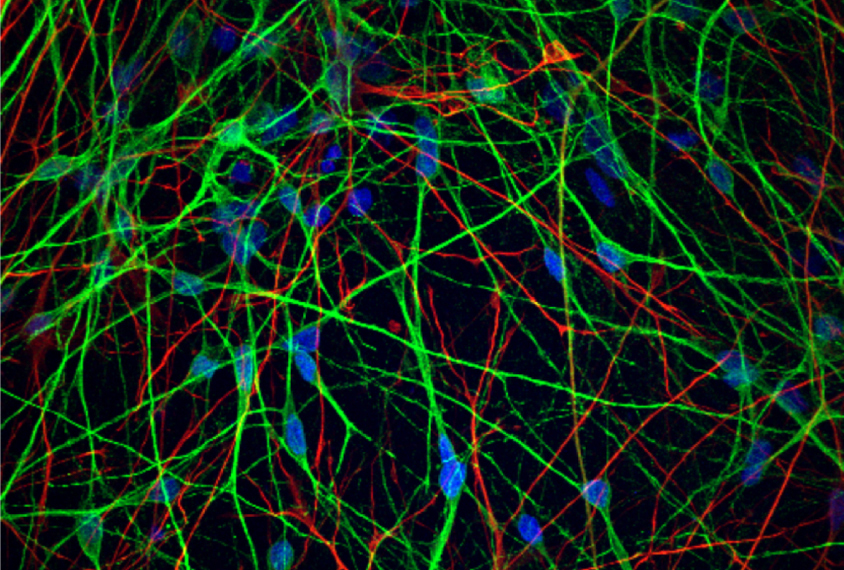
Courtesy of Rakhi Pal, Bharath Reddy and Sumantra Chattarji
A change in the proteins secreted by astrocytes, star-shaped cells that support neurons, may contribute to the atypical firing patterns of neurons in people with fragile X syndrome, according to a new study. The findings point to a possible target for treating the condition, which has so far eluded drug-development efforts.
“All our attention over the last couple of decades has been on trying to tweak neuronal mechanisms,” says study leader Sumantra Chattarji, director of the Centre for High Impact Neuroscience and Translational Applications at TCG Centres for Research and Education in Science and Technology in Calcutta, India. “This now opens up a framework for potential candidates that are astrocyte-based.”
Neurons derived from stem cells of people with fragile X syndrome fire more frequently, but in shorter bursts, than do control neurons, Chattarji’s team found in a previous study.
The new work shows typical neurons adopt this same firing pattern if they are cultivated with astrocytes derived from people with fragile X syndrome. And fragile X neurons don’t fire this way if they grow together with typical astrocytes. One of the causes seems to be a protein secreted by the astrocytes.
“The results are very clear, you know, very convincing,” says Yongjie Yang, professor of neuroscience at Tufts School of Medicine in Boston, Massachusetts, who has studied the role of astrocyte glutamate transporters and receptors in fragile X. The work confirms in human cells what Yang says scientists have “long suspected” based on mouse studies: “Actually, glial cells really play a significant role in modulating neuronal excitability.”
In the new work, Chattarji and his colleagues cultivated neurons and astrocytes from the stem cells of two people with fragile X syndrome and one without, whose cells served as a control.
Both fragile X neurons and control neurons grown with control astrocytes fire no differently than neurons typically do, Chattarji and his team found. “And then the ‘aha’ moment came,” Chattarji says: When either type of neuron grew with fragile X astrocytes, it fired atypically with shorter, more frequent bursts.
In other words, the astrocytes — not the neurons — determined the firing pattern. “I had no idea that astrocytes would become such a centerpiece of the story,” says Chattarji, who has previously focused mainly on neurons.
In his basic neurobiology class, Chattarji often lectures about a famous classic experiment by Otto Loewi: The scientist stimulated the vagus nerve of a beating frog heart, causing the beating to slow down. He then bathed another frog heart in liquid from the stimulated heart, causing the second heart to beat more slowly, too — and demonstrating that the signal was transmitted via chemicals in the liquid.
Using Loewi’s experiment as inspiration, the team bathed fragile X and control neurons in the culture media from both types of astrocytes. They saw the same results as before: Neurons bathed in the control medium fired normally, whereas those bathed in the fragile X medium had frequent, short-lived bursts. This meant that some chemical secreted by the astrocytes, and not their physical presence, was responsible.
An astrocyte-secreted protein called S100 beta is known to stabilize the firing of rat neurons, so Chattarji’s team suspected it might contribute to the fragile X neurons’ erratic firing. In support of this hypothesis, the team found that the concentration of S100 beta is lower than usual in the culture media of the fragile X astrocytes. Adding S100 beta to co-cultures of neurons and fragile X astrocytes normalized the neurons’ firing.
The mechanism seems to involve a phenomenon called the persistent sodium current, a small current that continues to flow through the neuron after it fires. Neurons bathed in the fragile X astrocyte media also show a lower-than-usual persistent sodium current; adding S100 beta increased it to normal levels, suggesting the protein could be a target for future treatments.
“This by no means suggests only S100 beta or the persistent sodium current are the only game in town,” Chattarji says. He says his team hopes to study fragile X astrocytes in more detail to understand how S100 beta is secreted; it’s not yet clear how it changes the persistent sodium current.
The new work is important because it adds to a growing body of research on fragile X “that tries to refocus people on thinking about how signaling from astrocytes might affect the disorder,” says Anis Contractor, professor of neuroscience at Northwestern University in Chicago, Illinois. “There has been a very neuron-centric view of the field.”
He and Chattarji both say that future research should seek to understand all the changes in astrocytes due to fragile X; for example, other research has revealed changes in metabolism, calcium signaling and the cell cycle in fragile X astrocytes.
It is also important to look beyond individual neurons and examine S100 beta’s effect on networks of neurons, Yang says. “That would be really exciting to see, whether that also can be rescued by the S100 beta.”
Cite this article: https://doi.org/10.53053/CHSN3730
This content was originally published here.