Microscopic electronic probes implanted within blood vessels in rats can record single-neuron activity without brain surgery, a new study finds.
The new devices may one day enable long-term minimally invasive recording deep within the brain.
“We could envision providing a quantum jump forward that may help to better understand the underlying brain factors important in autism,” says study investigator Anqi Zhang, a postdoctoral fellow in chemical engineering and bioengineering at Stanford University in California. Zhang says the technique could also help study the effects of medication on the brain.
Brain-monitoring devices typically involve trade-offs between how invasive and how sensitive they are. For instance, electroencephalography is noninvasive but cannot target individual neurons. It is limited to scanning neural activity at the brain’s surface. By contrast, recording single-neuron activity from deep within the brain often requires an invasive procedure to implant probes. Infection, inflammation and damage to brain tissues can result.
But with this new approach, Zhang and her colleagues demonstrated that they could record activity from the cortex and olfactory bulb through blood vessel walls down to the single-neuron level. The technique was less invasive than brain surgery, and the team detected no negative consequences to rodents’ health. Using this approach, they could pinpoint and monitor seizure activity induced by penicillin injections. (Epileptic seizures may occur in nearly half of individuals with autism.)
Though the probes have yet to be tested in people, “Accessing the brain via the vessels, as opposed to the skull, is likely a much more agreeable procedure to patients,” says György Buzsáki, professor of neuroscience at New York University, who did not take part in this research. He praised the work, noting that “the high-quality recordings are excellent, and the approach has promise.”
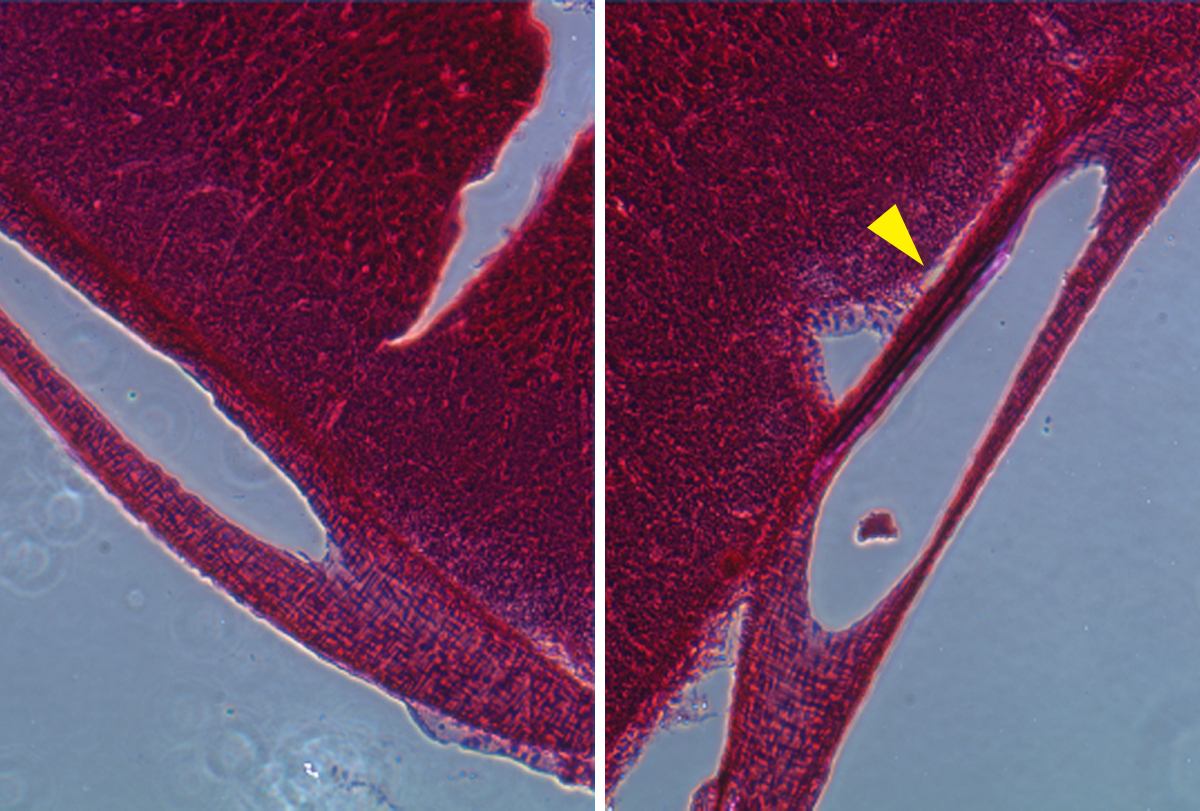
Embedded eavesdropper: The probe was able to record neuronal activity in the olfactory bulb of a rat.
In their study, Zhang and her colleagues designed a flexible mesh-like probe 900 microns wide with 16 platinum recording electrodes. They next rolled it up and loaded it within a flexible microcatheter.
A polymer guidewire helped the researchers bend the microcatheter to steer it into the dense network of blood vessels found throughout the brain. They expelled the probe using saline fluid and retracted the microcatheter, leaving the probe to unfurl. The electrodes were set in ribbons that stick to a blood vessel’s inner walls, enabling high-quality recording of nearby neurons, Zhang says.
Most neurons are located 10 to 20 microns from the nearest blood vessel, so these endovascular probes could theoretically access every region of the brain without intruding on its tissue. The researchers add that neurosurgeons already treat conditions such as artery thickening in the brain using stents implanted via incisions made in the jugular vein, carotid artery or other locations.
Despite the vessels’ fragility, the probes led to no substantial change in blood flow, immune response or rat behavior after 28 days of monitoring. Zhang and her colleagues published their findings last month in Science.
The long-term stability of this approach, together with the minimally invasive surgery needed to deliver it, “makes it highly promising for use in clinical applications in both neurological disease treatment and brain-machine interfaces,” says Sihong Wang, assistant professor of molecular engineering at the University of Chicago, who did not take part in this work.
Indeed, several researchers commented on how this work could be extended. “The platform demonstrated by the authors could be used to deliver micro- or nano-scale stimulation or recording elements nearly anywhere in the body, enabling new avenues for two-way bioelectronic communication,” says Brian Timko, assistant professor of biomedical engineering at Tufts University in Medford, Massachusetts, who did not participate in this research.
Previous research has used endovascular probes to record brain waves, but this earlier work mostly relied on stiff, bulky metal devices, limiting their use to blood vessels 2.4 millimeters wide. In contrast, the ultra-flexible probes employed in the new study could enter blood vessels less than 100 microns wide. (Prior work did develop flexible endovascular probes, but none reported tests in live animals.)
“If the technology allows large-scale recordings in the future, it has promises to offer a brain-wide view of global patterns,” Buzsáki says.
He notes that additional research should pinpoint where the probes’ electrodes end up to better interpret their data. However, this current uncertainty “does not detract from the fact that even in its current instantiation, the method provides a novel window on the brain.”
A key limitation of the probe is that it is only steerable for one branching point, whereas the vascular system has many branching points, Zhang says. “To address this limitation, we plan to incorporate magnetic materials at the tip of the probe and use magnetic fields to navigate it through many branches,” she says.
Future research can also explore making smaller probes that can enter even tinier blood vessels, as well as probes made from biodegradable materials that safely break down when no longer needed, Wang says.
Cite this article: https://doi.org/10.53053/UPPM4050
This content was originally published here.