The paper uses age and sex-matched subjects – one with ASD and one neurotypical (without ASD) – and analyses their microbiomes over a number of different studies.
The result was a conclusive pattern of differences between the microbiomes of ASD subjects and those of neurotypicals.
While it isn’t certain whether the microbiome causes ASD, or the reverse (for example, people with ASD are often picky eaters, less likely to consume foods high in glutamic acid, serine, choline, phenylalanine, leucine, tyrosine, valine and histidine, which may affect the microbiome), the fact that a connection exists is solidified by this paper.
This therefore opens up the possibility for future studies into this link that, when it is better understood, could lead somewhere down the line to microbiome-centred therapies to help people with ASD.
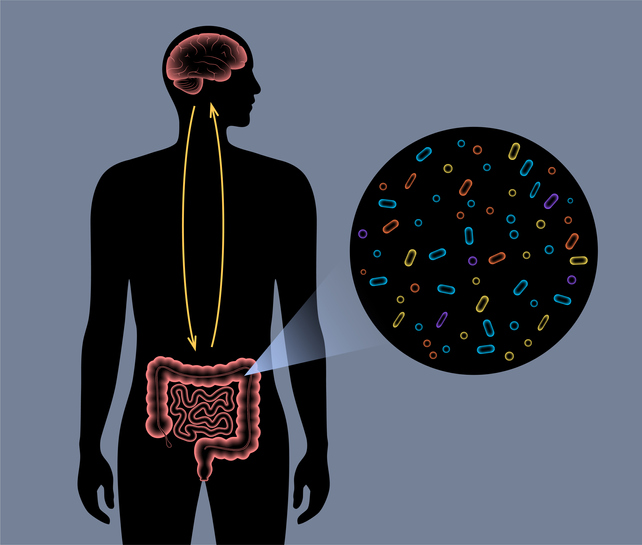
The gut-brain axis
There is little question of a link between the gut and the brain. “The gut-brain axis has been well established,” Gaspar Taroncher-Oldenburg, one of the paper’s authors, told FoodNavigator.
“There’s an ongoing and continuous communication between the gut . . . and the brain that goes in both directions. The brain can sort of modulate activity around the gut, and the gut in reverse can modulate the brain affecting mood and other things.
“More recently, the role the gut microbiome plays in the gut-brain axis has been studied, not just in the context of autism, but . . . in the context of the functioning of our bodies in general.
“Before we started studying the microbiome, we knew about the connection between the gut and the brain. Now we know that the microbiome can talk to the brain, so the connection is there.”
The limitations of previous studies
A range of literature has found a connection between autism and the microbiome. However, many of these connections were tenuous or not overlapping among studies. This, Taroncher-Oldenburg told us, is partially because of analytical limitations of studies, as well as their reduced sizes. While research showed clear differences between ASD subjects’ microbiomes and neurotypicals’, these were different differences, so to speak.
“But when you go from study to study, those differences are different, so there’s very little overlap.”
The uncertainty this creates means that, on the one hand, a lot of hype is created, and on the other, “it also creates a lot of room for people to doubt that there is a connection.”
One of the reasons for this is that the studies only represented a single snapshot in time. “There are many so-called cross-sectional studies that capture just one section in time, of both cohorts.
“So you don’t really know what came before, or what came after. All you know is that while you’re having the symptoms or whatever it is you’re measuring phenotypically, you know that you have this microbiome vs. that microbiome composition. That’s all you know. So it’s very hard to infer any kind of mechanistic insights from this, other than to say there is a difference in the microbiome.”
When studies of this kind are done, the cohorts of neurotypical and ASD subjects are carefully picked to match in age and sex. However, when it comes to analysing it, the data for each cohort of subjects is reduced to average.
Why is this a problem? A lot of information is lost this way. For example, “age is a huge component,” Taroncher-Oldenburg told us. “The microbiome in a seventeen-year-old is not the same as that of a four-year-old. And yet you only consider the average.
“When it comes to ASD phenotypes, we know that there is a big dichotomy in sex. You have a lot more boys, and with stronger symptoms than girls, and yet when mixed cohorts are analysed, the data from boys and girls are averaged, basically diluting the signal.”
Getting rid of the confounders of age and sex
In order to get rid of these so-called confounders, the researchers re-analysed cross-sectional data from existing cohorts by comparing subjects of the same age and sex directly. By not averaging out the results, they were able to discard the possibility that age and/or sex might be the real cause of the difference in the results, rather than ASD.
They also were able to substantially increase their dataset by now being able to compare data points across studies.
What they found when they did this was significant. “When we actually did the analysis that way, we saw that, lo and behold, you now could find very clear signals that were equivalent from study to study,” said Taroncher-Oldenburg, “simply by having done this, so all of a sudden you were seeing a much more homogenous readout.”
The results showed a clear continuity in the connection between differences in the microbiome and ASD in both the age and sex cohorts.
There was still a problem of time – their results simply represented a snapshot in time, not showing clearly that these differences would remain.
“In order for us to know if any of those signals were relevant or what they could mean, therapeutically or just in terms of disease, mechanistically, we needed to ‘ground-truth’ our results with longitudinal data, that had five or six data points over time that correlated with some kind of change in the autistic phenotype.”
Such a study that showed results over a number of years indeed existed. The study backed up their conclusions. While there is still a long way to go, some of their questions were answered.
“The goal of this was never and it still is not to find a list of ‘silver bullets’. There is not enough resolution for that. The existing studies were not designed that way.
“All we wanted to see is whether if we took a different look at existing data we could once and for all lay to rest hype or doubts surrounding the question whether the microbiome has anything to do with autism.”
While which way the link goes – whether a certain microbiome composition leads to autism, or the other way around – is not yet known, the link itself is nevertheless clearly established.
Changes in the microbiome could also be linked to diet. “When we look at metabolites – and metabolites are a reflection of diet – we do see how there are certain metabolites and groups of metabolites that correlate much stronger with ASD-specific microbiomes, and that signature is very strong,”
However, diet isn’t always easy to study. “Anything to do with diet is absurdly difficult to study, because self-reported, or somehow otherwise reported diet data, are very hard to come by.”
Still, diet and microbiome are inextricably linked, so of course the connection is there. It simply has not yet been studied to the full possible extent it could be.
Hoping for a better life
In the end, the impetus for the study, as for much of the field, is the possibility that understanding how the microbiome affects ASD could one day lead to a therapy that could help people with it.
“The very idea of looking at this is that down the line,” Taroncher-Oldenburg told us, “if you understand these mechanisms better, you might be able to design interventions through diet or diet plus probiotics or prebiotics or some kind of supplement that are non-invasive, but that could modulate the microbiome in not so subtle or subtle ways to then influence behaviour and have a positive outcome in kids with autism.”
He stressed that “when you talk about autism, and this is something that is very important to understand, at no point is anybody thinking about manipulating the microbiome through diet or another way such that you’re going to cure autism.”
A therapy, however, could help people with ASD. “Something that is not going to cure but it’s going to improve the symptoms, and really that’s what most families are looking for.”
Sourced From: Nature Neuroscience
‘Multi-level analysis of the gut–brain axis shows autism spectrum disorder-associated molecular and microbial profiles ’
Published on: 26 June 2023
DOI: https://doi.org/10.1038/s41593-023-01361-0
Authors: J. T. Morton, D. Jin, R. H. Mills, Y. Shao, G, Rahman, D. McDonald, Q. Zhu, M. Balaban, Y. Jiang, K. Cantrell, A. Gonzalez, J. Carmel, L. M. Frankiensztajn, S. Martin-Brevet, K. Berding, B. D. Needham, M. F. Zurita, M. David, O. V. Averina, A. S. Kovtun, A. Noto, M. Mussap, M. Wang, D. N. Frank, E. Li, W. Zhou, V. Fanos, V. N. Danilenko, D. P. Wall, P. Cárdenas, M. E. Baldeón, S. Jacquemont, O. Koren, E. Elliott, R. J. Xavier, S. K. Mazmanian, R. Knight, J. A. Gilbert, S. M. Donovan, T. D. Lawley, B. Carpenter, R. Bonneau & G. Taroncher-Oldenburg
This content was originally published here.