In 2009, Mark Shen noticed something odd in the brain scan of a 6-month-old who had an older sibling with autism: excess fluid between the brain and the skull. Shen — then a graduate student in David Amaral’s group at the University of California Davis MIND Institute — and his colleagues set out to quantify the amount of brain fluid from the scans of younger siblings of children with autism. Such ‘baby sibs’ have a 20-fold higher chance of having the condition compared with the general population.
Six-month-old baby sibs who went on to be diagnosed with autism had, on average, more brain fluid than controls, the team reported in 2013. Since then, Shen and his collaborators have confirmed the link between excess brain fluid and a later diagnosis of autism in hundreds of infants, including some who have no family history of autism.
The buildup of fluid could provide clues to the biological basis of autism, says Geraldine Dawson, professor of psychiatry and behavioral sciences at Duke University in Durham, North Carolina, who was not involved in the research. Cerebrospinal fluid (CSF) — the nutrient-rich solution surrounding the brain and spinal cord — contains growth factors that control neuronal proliferation, and it may clear metabolites that can influence early brain function and development.
Excess CSF is already associated with developmental delay and motor deficits, and alterations in CSF production and turnover have been observed in Alzheimer’s disease and other age-related neurologic conditions characterized by cognitive and motor difficulties.
Shen, now assistant professor of neuroscience and psychiatry at the University of North Carolina at Chapel Hill, is trying to understand whether defects in CSF circulation might also contribute to autism. Studies in people and animal models — much of these still unpublished — suggest that the excess fluid could also occur in autism-linked syndromes. The accumulation may even be tied to sleep problems, which have been reported in up to 80 percent of children with autism.
The research is still in its infancy, and it isn’t straightforward. But if it pans out, excess CSF may eventually be used to predict autism likelihood in infants, so long as it’s combined with additional information about the child, Dawson says.
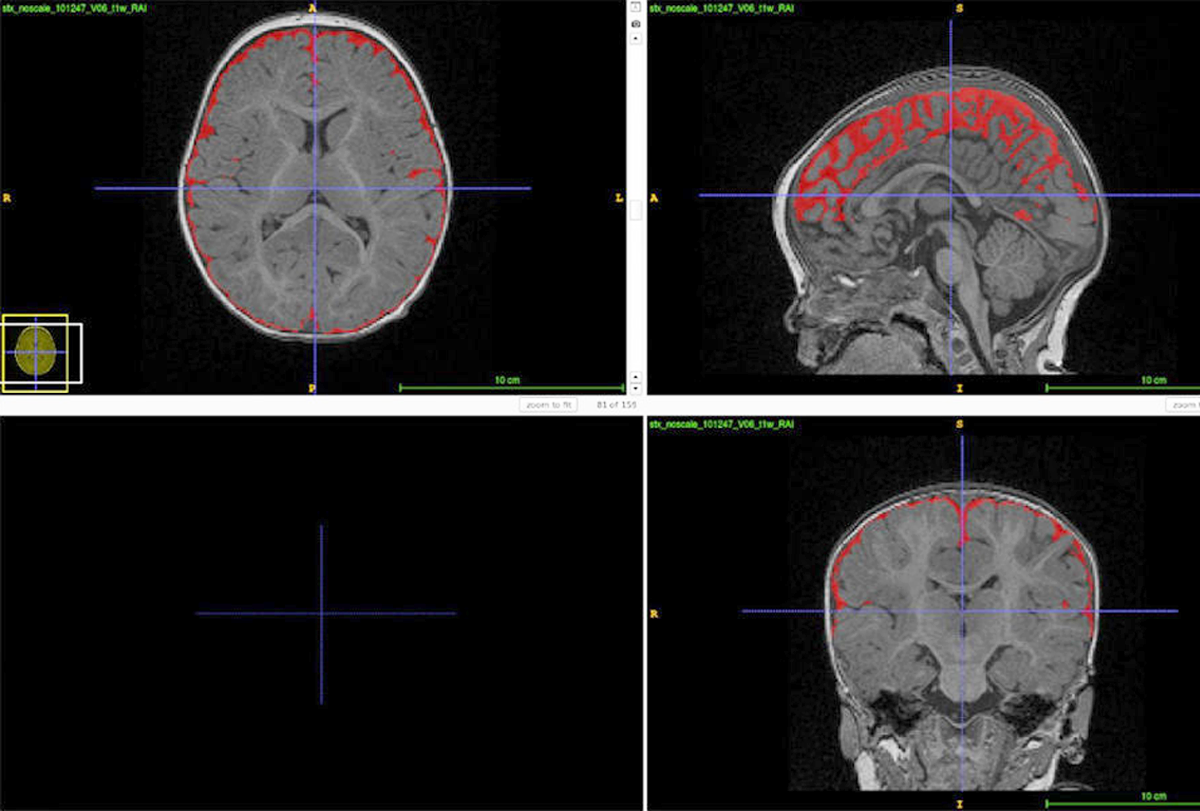
Brain swell: A 6-month-old infant who was later diagnosed with autism (bottom row) had excess cerebrospinal fluid surrounding the brain (depicted in white) compared with a typically developing infant (top row).
Every day in a typical adult, the cells lining the fluid-filled spaces in the brain produce about half a liter of CSF. And that fluid turns over three or four times over the course of 24 hours — primarily during sleep — although these numbers may be different in infants. As it moves across the brain, CSF collects neuronal waste products and inflammatory molecules — including some linked to autism and Alzheimer’s disease — and flushes them into the body’s circulation. “We like to refer to it as the plumbing system of the brain,” Shen says.
Even though it was a small study, 8 of the 10 baby siblings in Shen’s initial analysis who were later diagnosed with autism had significant CSF backflow — with about 20 percent more fluid on average than 34 neurotypical children and 11 children with general developmental delay assessed using MRI at 6 to 9 months of age. And the more fluid autistic children had at 6 months, the more motor delays they showed later in infancy, according to a larger 2017 follow-up study Shen led.
To understand whether, and how, a buildup of brain fluid may contribute to autism, his team has since turned to rodent models of fragile X syndrome, the most common inherited form of autism. Like the baby sibs, these model animals have more brain fluid compared with controls. They also show less CSF circulation across the brain, according to unpublished results Shen presented in May at the annual meeting of the International Society for Autism Research (INSAR). (Links to INSAR abstracts may work only for registered conference attendees.)
The sluggish circulation may overexpose the developing brain to harmful molecules, Shen says. In support of this idea, the fragile X models have a reduced ability to clear out inflammatory proteins from the brain, unpublished work from Shen’s lab suggests.
Shen’s hypothesis sits well with the scientific literature, says Cara Westmark, assistant professor of neurology at the University of Wisconsin-Madison, who was not involved with the research. Mice with reduced CSF flow are less able to flush out amyloid beta, the protein that coalesces into large plaques in the brains of people with Alzheimer’s disease, a 2012 study found.
Amyloid beta levels are similarly increased in fragile X mice, according to work by Westmark and her team. The protein and its precursor (APP) may also be elevated in the brains and blood of autistic people, studies have found.
“[It] makes sense that if the brain is unable to clear out these proteins, […] that would cause problems with neuron function,” Westmark says. However, she adds, it remains to be determined if alterations in CSF flow are a cause or a consequence of autism.
The buildup of amyloid beta can alter synaptic transmission, trigger neuronal injury and disrupt neuronal networks, according to studies in animal models and neuronal cultures. But there’s “tremendous” skepticism, at least in the Alzheimer’s field, about whether amyloid beta is causing disease in people, says George Perry, professor of neurobiology at the University of Texas at San Antonio.
In the past two decades, most clinical trials of amyloid-targeted therapies for Alzheimer’s disease have failed. Perry’s research suggests that amyloid beta helps neutralize chemicals that can harm brain cells. Amyloid beta “is a normal protein that plays a critical role in brain function,” Perry says.
Even so, “too much of a good thing can be bad,” he adds. Therefore, measuring its levels in children with autism, and understanding how the protein moves from where it’s produced to where it’s cleared out would be important, he says.
In infants later diagnosed with autism, CSF buildup is associated with sleep disturbances, Shen and his collaborators reported in 2018. Most children with autism have disrupted sleep, and sleep problems are twice as common among autistic children as they are among neurotypical children. Shen’s team is now conducting a longitudinal study to try to discover whether CSF alterations precede or follow sleep difficulties in children with the conditions.
“We know that the majority of CSF turnover and movement is taking place during sleep,” says A.J. Schwichtenberg, associate professor of human development and family science at Purdue University in West Lafayette, Indiana, because it is linked to “slow wave” oscillations. “The slow-wave oscillation happens first and then, shortly afterwards, you see a pulse of CSF,” says Schwichtenberg, who wasn’t involved in Shen’s studies.
“We have reasons to believe that having sleep problems is linked with [worsened] CSF movement,” she adds. Even one night of sleep deprivation can reduce the brain’s ability to clear out waste products, a 2021 study showed, leading to increased levels of amyloid beta in CSF and the brain itself. Sleeplessness can also boost levels of tau, a protein linked to autism and Alzheimer’s disease.
“Sleep problems are comorbid with autism and Alzheimer’s disease,” Westmark says. “These findings support the hypothesis that poor clearance of waste products from the brain contributes to neurological impairment.”
Regardless of its underlying biology and link with sleep, a build-up of CSF holds the potential to be an early indicator of autism, Shen says — provided scientists find ways around some important limitations. Knowing which infants are most likely to have autism would enable clinicians and parents to get an early start on behavioral interventions, which, research suggests, may be most effective when started before age 2 and a half.
An algorithm combining different measures (including sex, age, excess CSF and brain volume at 6 months of age) predicted which baby siblings were later diagnosed with autism with about 70 percent accuracy, Shen’s work has shown. However, excess brain fluid doesn’t forecast autism with absolute certainty, says Jared Nielsen, assistant professor of cognitive and behavioral neuroscience at Brigham Young University in Provo, Utah.
By itself, CSF volume may not be enough to make predictions with a clinically meaningful level of certainty; researchers would need to combine it with other brain measurements or behavioral traits, Nielsen says. “We need maybe more complicated algorithms that combine lots of sources of information and not just the amount of fluid that’s surrounding the cerebral cortex.”
The usefulness of CSF as a biomarker could be limited in other ways: its buildup occurs in autistic children up to age 3 but not in older autistic children and adults, according to two studies Nielsen led. And the precise rate of CSF production and absorption in infants and toddlers is unknown, Shen says. “There is some old literature suggesting that CSF production in infants is faster but absorption is slower than in adults.”
To make excess brain fluid work as a biomarker for autism, researchers would also need to determine how specific this trait is to the condition. Children at high risk for schizophrenia do not show signs of CSF accumulation outside the brain, according to a 2020 study. But excess fluid is present in infants with Angelman syndrome, a rare genetic condition linked to autism, and those with fragile X syndrome, according to Shen’s INSAR 2023 presentation.
Excess CSF may be specific to autism, but Shen’s findings need to be replicated in larger studies, says John Gilmore, director of the Center for Excellence in Community Mental Health at the University of North Carolina at Chapel Hill. MRI and other brain imaging techniques have gained attention as ways to identify biomarkers for autism, but “nothing has really panned out over the years.”
If excess CSF and the inability to clear out neuroinflammation are present in only some autistic people, that may help researchers parse the condition into subtypes, Shen says. Identifying specific autism subgroups, he adds, “offers the possibility down the road to develop more targeted therapies.”
Ultimately, he adds, understanding how the accumulation of brain fluid is linked to autism will require assessing CSF production and turnover, and analyzing the fluid’s content in young children. Both are difficult to do. CSF can be collected only through an invasive procedure known as a spinal tap, and using MRI to study CSF absorption requires the injection of tracer chemicals — a method that researchers wouldn’t use repeatedly in young children, Shen says.
“I haven’t lost all hope that CSF volume is some sort of biomarker [for autism],” Nielsen says. “But there’s still a lot of work that needs to be done.”
This content was originally published here.