An altered eye reflex may distinguish children with mutations in SCN2A, one of the genes most strongly linked to autism, according to a new preprint.
The simple test the researchers used to analyze the reflex “may be a useful clinical biomarker of SCN2A-related autism,” says Alfred George, professor and chair of pharmacology at Northwestern University in Chicago, Illinois, who was not involved in the work. “This has potential uses for diagnosis and as a ‘read-out’ for therapies.”
Mice with a mutation in SCN2A also show the altered reflex, which became more typical after the researchers counteracted the mutation’s effects in adolescent animals.
This “gives us some hope that, if and when such a therapeutic gets into clinical trials, it may be beneficial, even for those kids that have lived with an SCN2A disorder for quite a while,” says co-lead investigator Kevin Bender, associate professor of neurology at the University of California, San Francisco.
Up to 90 percent of autistic children have atypical responses to sensory stimuli. Research into the neural circuitry behind these sensitivities has generally focused on the forebrain, which holds the brain’s main sensory processing centers. But such sensitivities may also involve reflexes that kick in before sensory information reaches the forebrain, according to a 2015 study.
The new study investigated the vestibulo-ocular reflex, which helps people keep a steady gaze whenever their head moves, triggering eye movements in the opposite direction of the head. In neurotypical children, this reflex is sensitive to fast head movements but less so to slower ones, whereas in autistic children it tends to be sensitive to both fast and slow movements.
To measure this reflex in 5 children with loss-of-function variants in SCN2A and 11 neurotypical children, Bender and his colleagues developed a lightweight, helmet-mounted infrared eye-tracking system paired with motion-detecting electronics. The children wore this apparatus while turning back and forth on a swivel chair, revealing that the reflex differs between those with and without SCN2A mutations.
Similar differences turned up between SCN2A mice and wildtype mice placed on a rotating platform outfitted with an eye-tracking device. “We could see differences between animals with SCN2A loss and littermates that had normal SCN2A levels, just by looking at how their eyes moved in response to a movement of their head,” says co-lead investigator Guy Bouvier, a group leader at the Paris-Saclay Institute of Neuroscience in France.
Mice lacking a copy of SCN2A have previously shown few clear changes to behaviors such as social interaction and repetitive behavior, Bender says. “By contrast, eye movements in these mice were dramatically different. It’s the most robust behavioral effect we’ve ever seen in the lab.”
Neuronal activity in the cerebellum mediates the vestibulo-ocular reflex, previous studies suggest. Mice engineered to carry a loss-of-function SCN2A mutation in cerebellar granule cells show alterations in synaptic plasticity, the new study found.
Specifically, the mutation impaired plasticity between granule cells and Purkinje cells, which connect the cerebellum to other brain areas. This, in turn, prevented synaptic changes that would typically adjust the vestibulo-ocular reflex’s sensitivity. The scientists posted their findings on the preprint server bioRxiv in June.
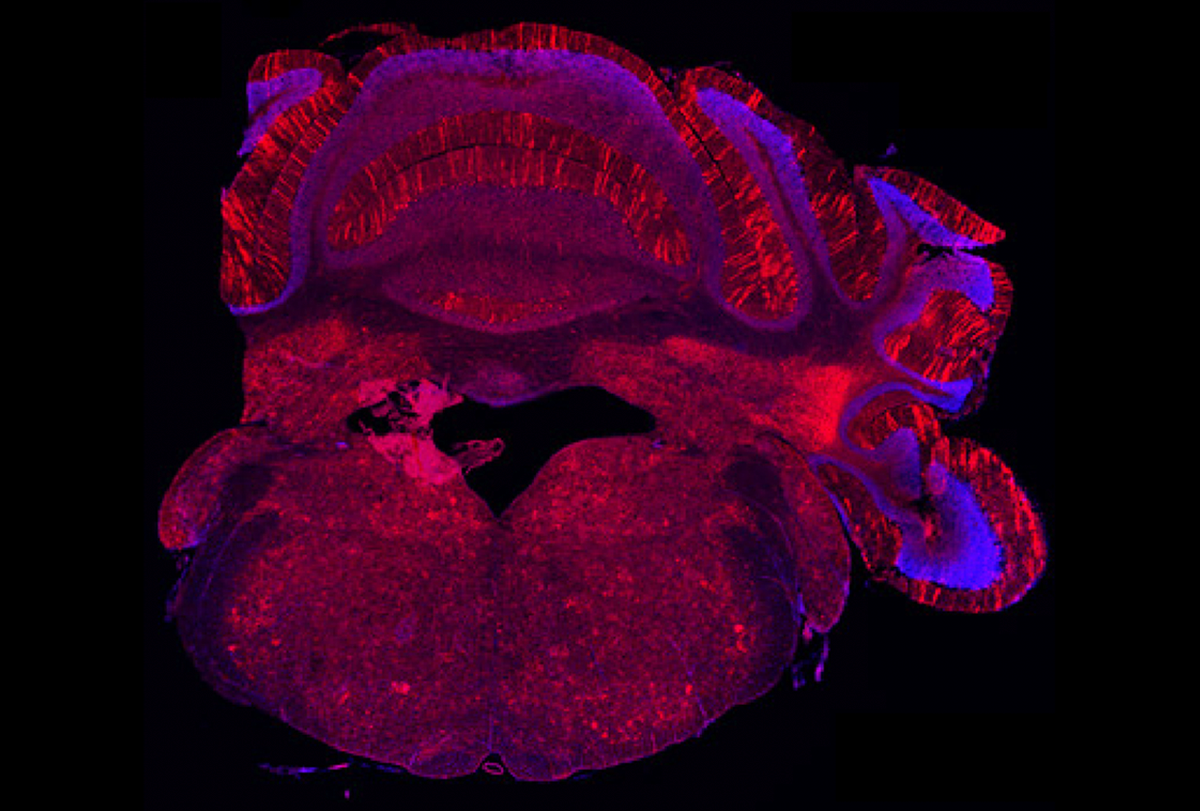
Involuntary actions: Some neurons in the mouse cerebellum express SCN2A (green) and help control the eye reflex.
“We think this highlights a role for the cerebellum in autism spectrum disorder that is a little less appreciated than it should [be],” Bouvier says. “Autism affects the entire brain, and the cerebellum interconnects heavily with social and emotional centers.”
Adolescent SCN2A mice showed typical plasticity for the reflex after the scientists used a CRISPR-based approach to boost SCN2A expression. This may raise hopes for a human version of this therapy, “but it’s going to take some time before we are really at that moment,” Bender says.
Children with SCN2A loss-of-function mutations typically speak few or no words and have difficulty following instructions. “The newly developed vestibulo-ocular reflex testing paradigm appears to be straightforward to implement, even in patients who are nonverbal or uncomfortable with restraint,” says Stephanie Rudolph, assistant professor of neuroscience, psychiatry and behavioral sciences at the Albert Einstein College of Medicine in New York City, who did not participate in this work. “It should be determined at what stage of development vestibulo-ocular reflex testing can be evaluated in patients.”
Future research should investigate whether the atypical reflex manifests in children with other conditions. “There are hints that it might be more common, but a much larger group of kids need to be studied to know for sure,” Bouvier says.
It remains unclear whether alterations in this reflex contribute to other aspects of autism, Rudolph notes. Still, testing whether adjusting the reflex “improves other behavioral deficits in SCN2A mice is an enticing possibility that should be explored,” she says.
This content was originally published here.